Jump links within this page:
Links to more tummy tuck experience pages on this blog:
- Abdominoplasty (page 1 of 7)
- On the Inside (page 2 of 7)
- Life Happens (page 3 of 7)
- The Decision (page 4 of 7)
- Surgery (this page)
- Initial Healing (page 6 of 7)
- Recovery (page 7 of 7)
To Everything There Is a Season
The projected recovery time for patients undergoing abdominoplasty plus liposuction ranges from 3-6 months. I planned my procedure for October so that, if my recovery is brief, I will be free to travel and escape the dark Oregon winter at the start of the year. And if, on the other hand, my convalescence takes longer, I’ll rejuvenate along with the rest of Earth’s northern hemisphere as spring approaches.
Preparations for the Long Season
Pre-op Medical Appointment
With the initial consultation behind me, I asked my bestie to accompany me to the pre-op visit. Her presence was critical not only for empathy and moral support but, from a cautionary perspective, I felt it was imperative that we each heard and understood the doctor’s instructions. Indeed, two heads are better than one.
We reviewed my medical history, I was examined, and my “before” pictures were taken. We discussed in depth the planned procedures, anesthesia, and potential risks. We reviewed the steps I would take in preparation for surgery and the ensuing post-operative period of time. Dr. Fichadia shared her expertise in her characteristic kind, confident, and warm manner. I left the clinic with a folderful of tips, instructions, and a copy of my consent forms.
At home, I studied the packet, made copious notes, and phoned the clinic with follow-up questions. As the day of the operation neared, I felt I knew what to expect, what to do, what to buy, what’s required, and what’s optional.
Financial
Elective procedures are rarely covered by insurance and, therefore, paid in advance and out-of-pocket. I decided to help myself out by securing a sizable discount. Here’s how: U.S. credit card providers offer tempting cash-back promotions to attract new customers. Basically, the game is that you agree to open a new account and spend in excess of a set dollar amount within a given period. In return, the card provider rewards you with cash, points, miles, or similar. In this instance, I was looking for cash rewards that would offset the costs of my surgery.
I weighed the pros and cons of the temporary damage to my creditworthiness that would surely result from opening several new credit lines at once, and then I did it anyway. With 3 upcoming huge purchases—the doctor’s, anesthesiologist’s, and hospital fees—I was confident that I would breeze past the card companies’ spending targets, and secured a naughty number (not telling you how many!) of accounts. By strategically splitting purchases across the newly attained cards, I fulfilled the respective conditions within days of activation and earned upwards of $200 in bonus dollars per card. And by paying off the entire credit card debt within 30 days, I paid no service fees whatsoever.
Domestic
On the post-operative pain spectrum, I expected I’d be somewhere between uncomfortable, at the very least—if not in agony, at most. My post-op instructions prohibit activities like lifting, straining, and reaching for a time. During sleep, I am to keep my knees flexed and restrict my orientation. Although stairs should not present a problem, I decided to move out of my bedroom and set up in the ground-level living room, closer to the kitchen and front door. I also wanted to sleep on the living room sofa and not my bed. The supportive sofa’s comfortable, yet confined, space was ideal for sidestepping the temptation to roll over and reposition during the night.
To make my stay more comfortable, I brought down clothing, medications, supplements, personal hygiene items, a bed tray, and laptop computer. Here’s the full itemization:
- A variety of loose, comfortable clothes
- Panty liners
- Slippers
- Eye glasses
- Eye cream
- Medications and supplements as directed
- Electric toothbrush/flosser
- Toothpaste
- Soap
- Cell phone charger
- This unique tray*
- Laptop computer/charger/external mouse
___________________
* Warning: If not handled gingerly, this particular tray can pinch the skin. Keep away from children.
I cooked, packed, and stored mounds of protein-rich foods like chicken and steak. I ensured that the fridge was filled with fruits and veggies that I enjoy, and that the freezer was jam packed with bagels. I posted a sheet detailing my food preferences—how I like my eggs, what goes on my bagel, which fruits I like best, how to warm up the pre-cooked steak and chicken, etc. This freed me to make simple requests like “please make me a bagel” without the need to clarify further.
Surgery
When it was time, I modified my diet and habits per doctor’s instructions, starting on some supplements and increasing my protein intake, but then fasting the night before surgery. On the eve prior to the big day, I also went to bed early so that I would wake up fresh.
Check-in
Check-in at the hospital was at 7 a.m. From the moment I was picked up at the house, I could not stop talking the entire drive to the hospital. I heard myself—but couldn’t stop myself. I believe this is referred to as logorrhea, which overwhelms me from time to time.
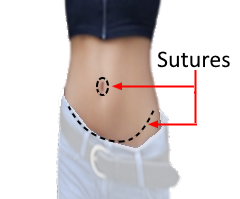
My incessant, nervous chatter continued as I made my way through the hospital. There was lots to accomplish in the 90 minutes prior to the scheduled surgery time of 8:30 a.m.: wardrobe changes, body art (i.e., pre-operative markings to guide the surgeon), and last-minute advice. My ongoing logorrhea indicated that, by this time, I was not my best self. To get through the day, I dissociated from the world around me. I barely noticed the thick, black lines Dr. Fichadia added to my mid-section, though I did register my bestie’s eyes widen as she looked on. By this time, I had become disengaged, not even taking a moment to consider and say “good bye” to her, or to the body I knew. Although it is deeply dispiriting and unempowering, dissociation is my go-to tactic that enables me to endure difficult situations. With continued efforts, perhaps I will evolve and assume strategies to remain present and better face hardship.

From the nursing team came the temperature and vital sign checks, lots of questions, and the dreaded poking—to find a vein, that is.
My defiant veins routinely shy away from a well-aimed instrument, a phenomenon that regularly presents a problem at blood draws, donations, and before surgery. I encouraged the nurse to limit her attempts to find a vein. The team’s established protocol is that, if she is unsuccessful in securing the line at two separate sites (like the forearm and the hand), she is urged call in an expert phlebotomist who handles difficult cases.
Advocacy in a Medical Situation
Into the madness entered a determined anesthesiologist. Undeterred by the chaos and my pained expression, he ran through his script and I did my best to comply. But when I couldn’t continue and asked him to give us a moment to finish, he declined; something about a timeline. He was determined to get my feigned agreement and signature. And I was afraid to piss off a man who held life and death power over me. I do wish someone had spoken up on my behalf (“hey, man, the lady asked for 5 minutes!”), as I felt incapable. It also would have been better had I waited him out by simply ceasing to interact. Or he could have just been compassionate.
I am not wired to advocate for myself as I would if it were for you. I came prepared to handle the IV situation, knowing I am entitled to request a second phlebotomist. And indeed, after the two excruciating yet unsuccessful pokes, my nurse called in the phlebotomy fairy (another nurse) who barely touched me with her magic wand (needle) and—poof!—the IV was in.
But I was not ready to singlehandedly field the badgering anesthesiologist. Had he respected my wishes, left, and then returned, nothing will have been lost.
Showtime
With a clean IV drip on my right hand and a medicinal cocktail to knock me out, I went out like a light and was wheeled into surgery in no time. The operation, scheduled for 8:30 a.m., was estimated to last 3-4 hours. Things went well, I’m told, and the procedure ended well ahead of schedule at about 10:30 a.m
Major Steps of a Full Abdominoplasty



Backstage
I awoke in the recovery room and asked whoever was tending to me: “are we done here?”—because that’s what I always ask after waking up from anesthesia. I was told that yes, we are done. I was probably offered water or medication, but I honestly don’t remember.
Resting comfortably, I admired my well-tailored abdominal compression garment that had been placed on me during surgery. This garment (or its duplicate, thoughtfully included in my to-go bag) was to remain on my person for 23.5 daily hours for the next few weeks. Extending from my midsection was a rubbery tube with a globe attached at one end. Or, to use medical terms, I was connected to a single surgical drain at whose end was a Jackson-Pritt collection bulb.
I suppose that the factors responsible for shortening the duration of my surgery by several hours are the same as those that made me a good one-drain candidate. Though it is typical for most patients, Dr. Fichadia informs that I just didn’t need a second drain installed.
My bestie arrived at 11:30 a.m. to find me “awake but groggy,” leading me to suspect that Mr./Dr. Heavyhanded doled out the anesthesia generously. I felt no pain, but was extremely thirsty, and remember going through 6-8 paper cups full of water in no time. To eat, I was offered two flavors of pudding and chose chocolate—duh! This, I do not remember, though.
My bestie patiently lingered for several hours as I recovered. A patient is discharged only after their vital signs are stable, they are sufficiently mobile, their pain and anesthesia-induced nausea are under control, and some other requirements are met.
When it was time to leave, I had nearly forgotten about my surgical drain since it was hanging on the drip stand, out of my view. I was given a large safety pin with which to attach the bulb to my special garment. I was to walk, talk, and sleep with this tube and bulb hanging out of me, which I still find absolutely bizarre.
I saw no reason to change into the clean clothes that I brought. Perhaps this is due to my compression garment looking like Wonder Woman’s evening wear. I was more than comfortable in my paper hospital gown and an overcoat. In fact, I asked for a second gown to take home. Best move I made that day!
➔ Advance to the Initial Healing page
